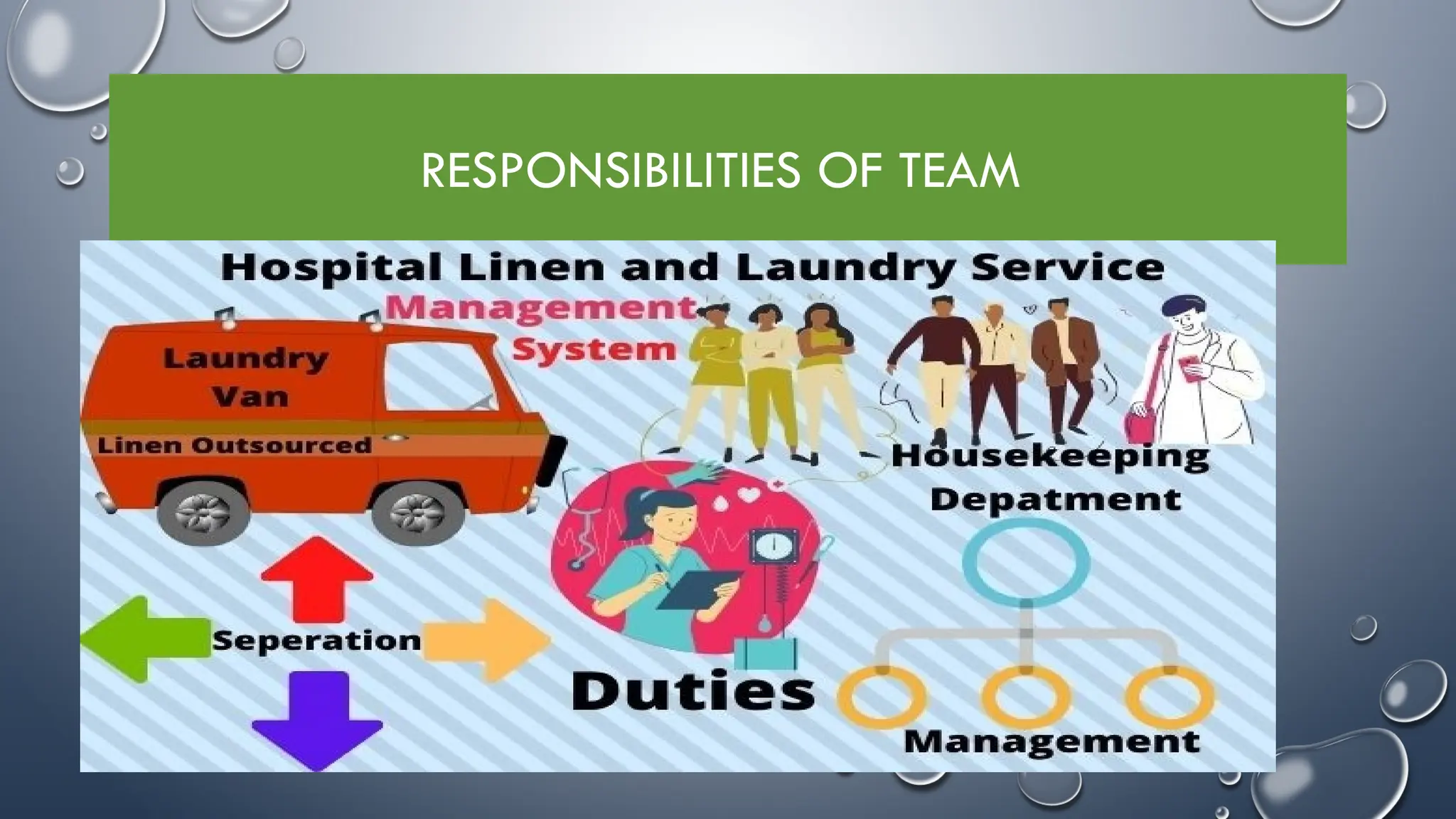
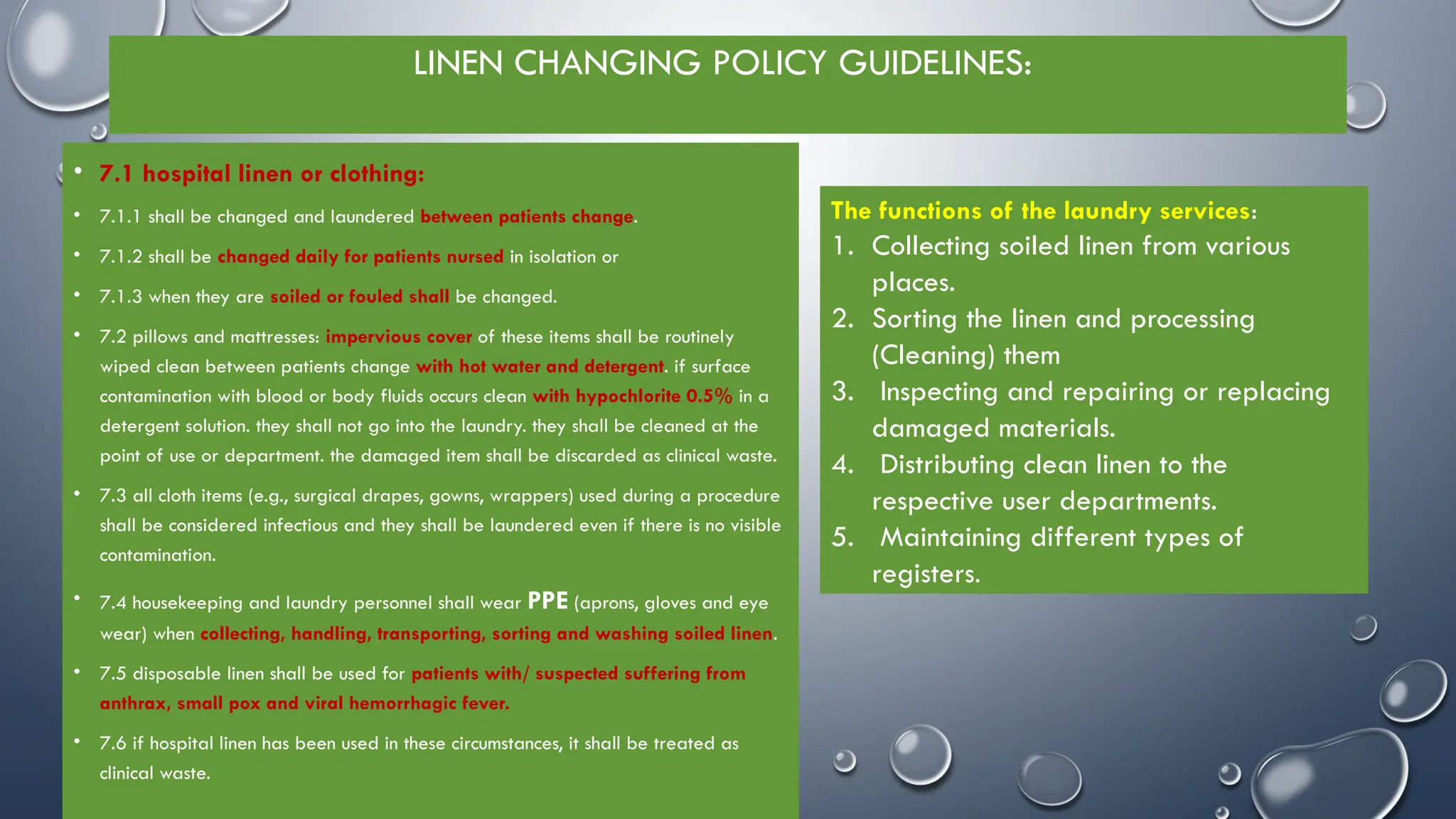
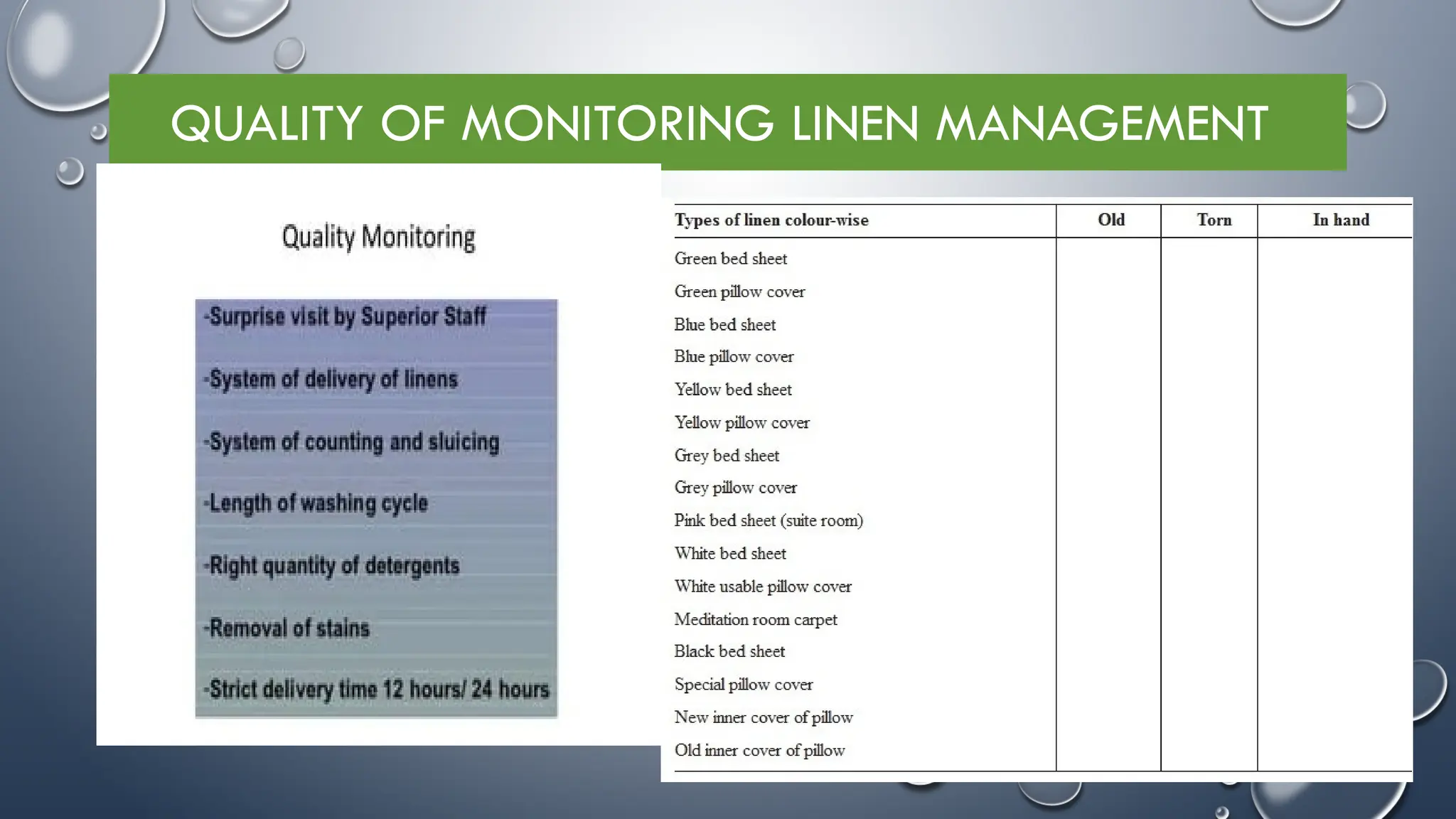
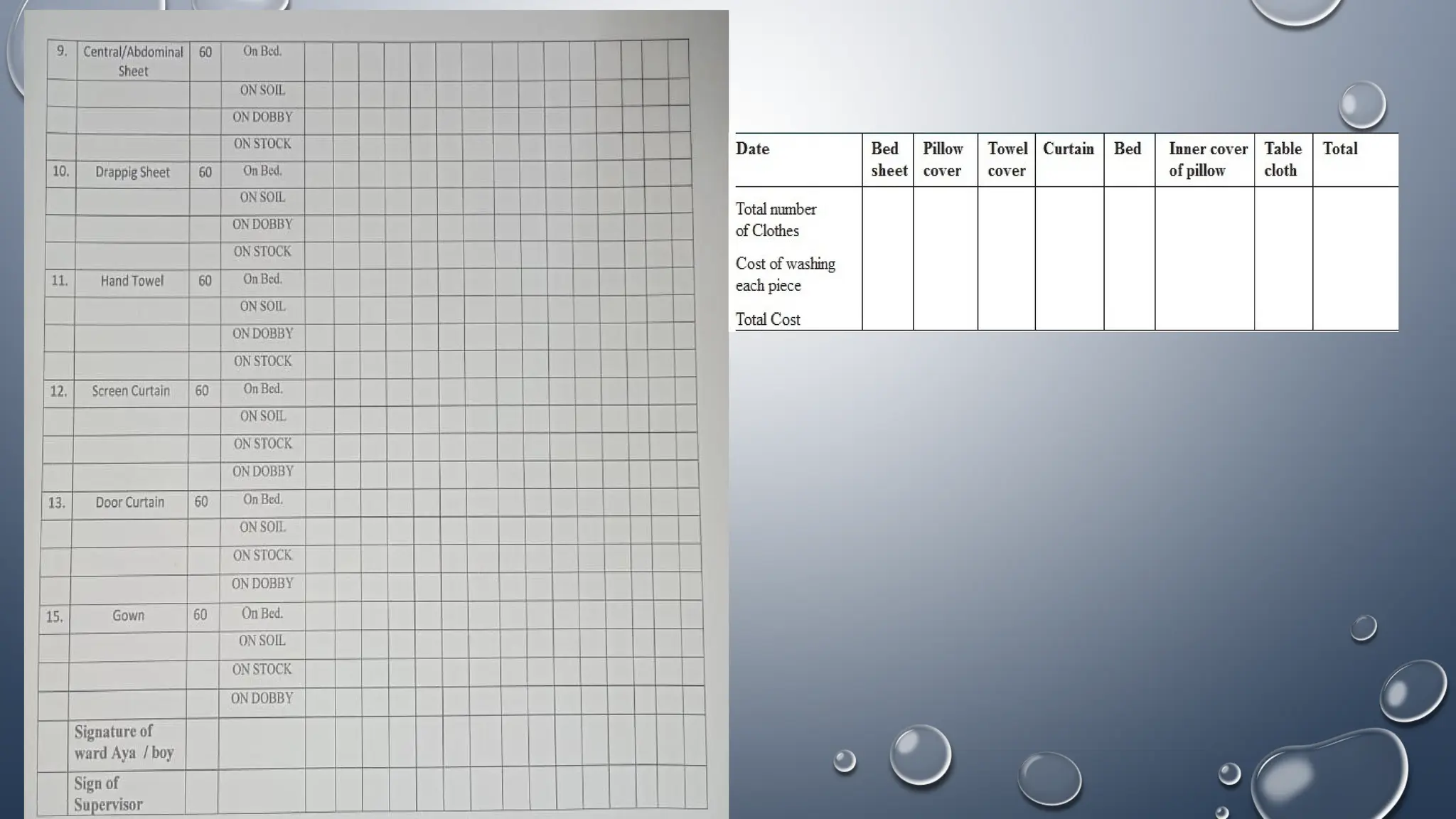
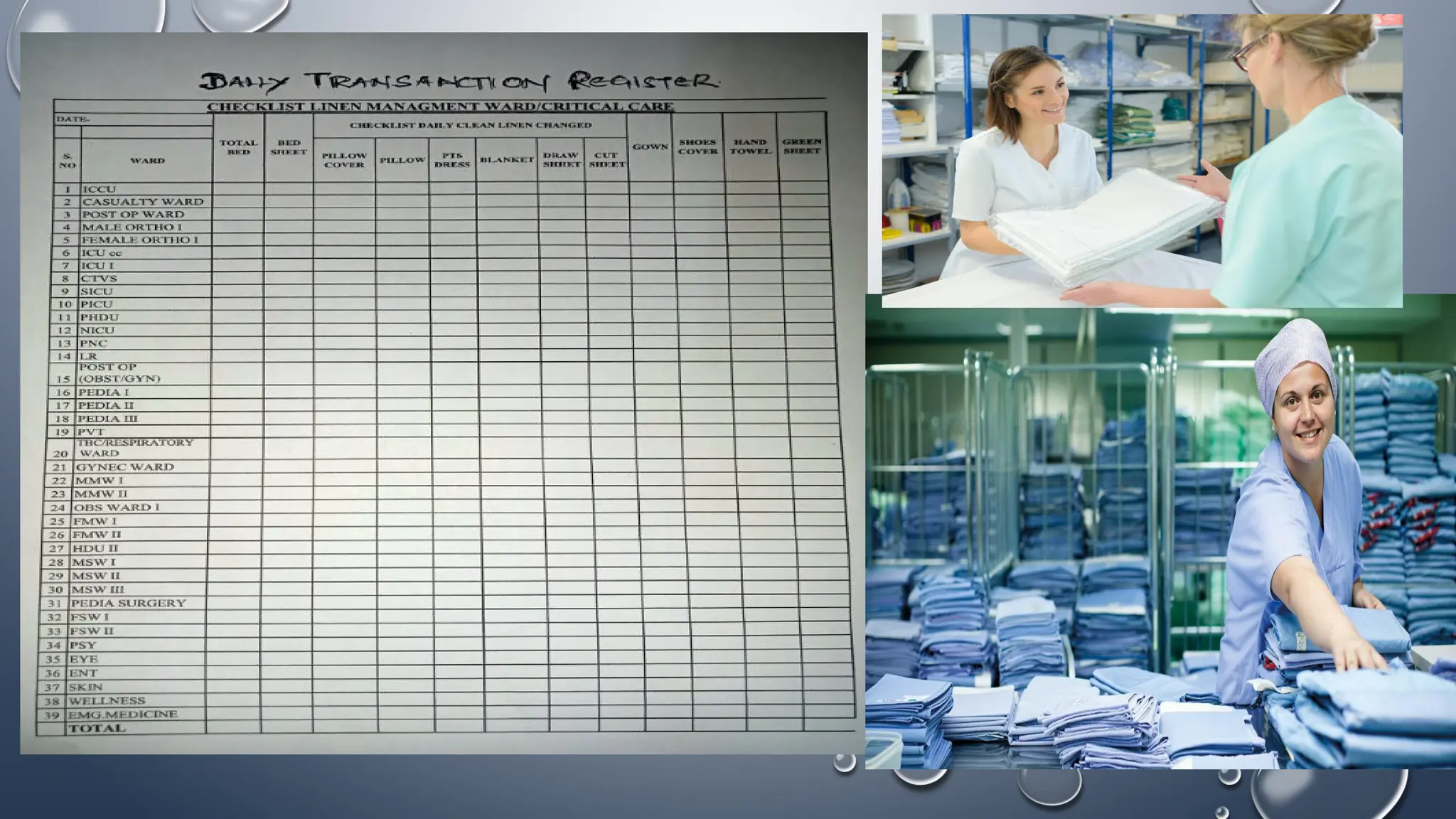
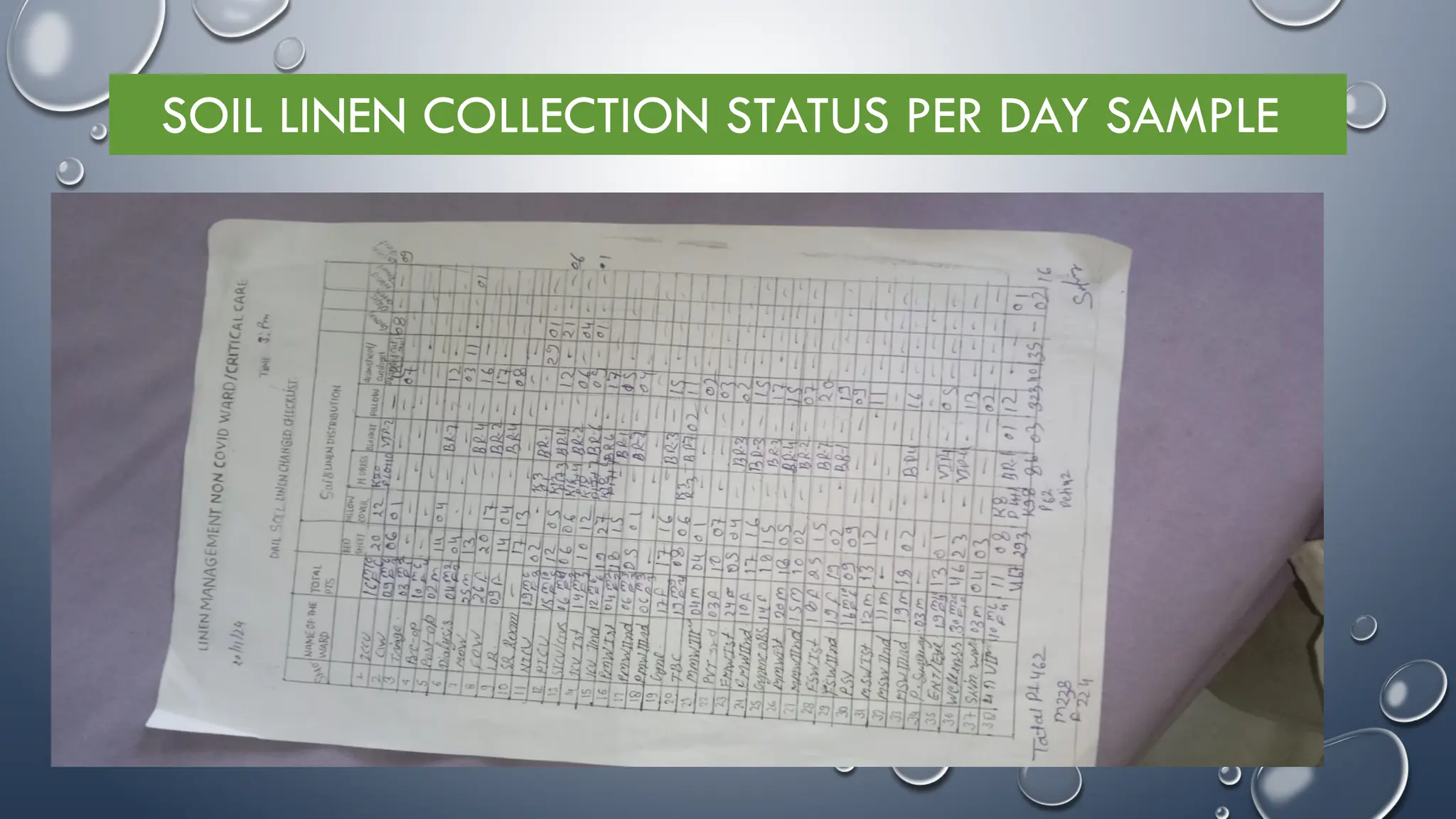
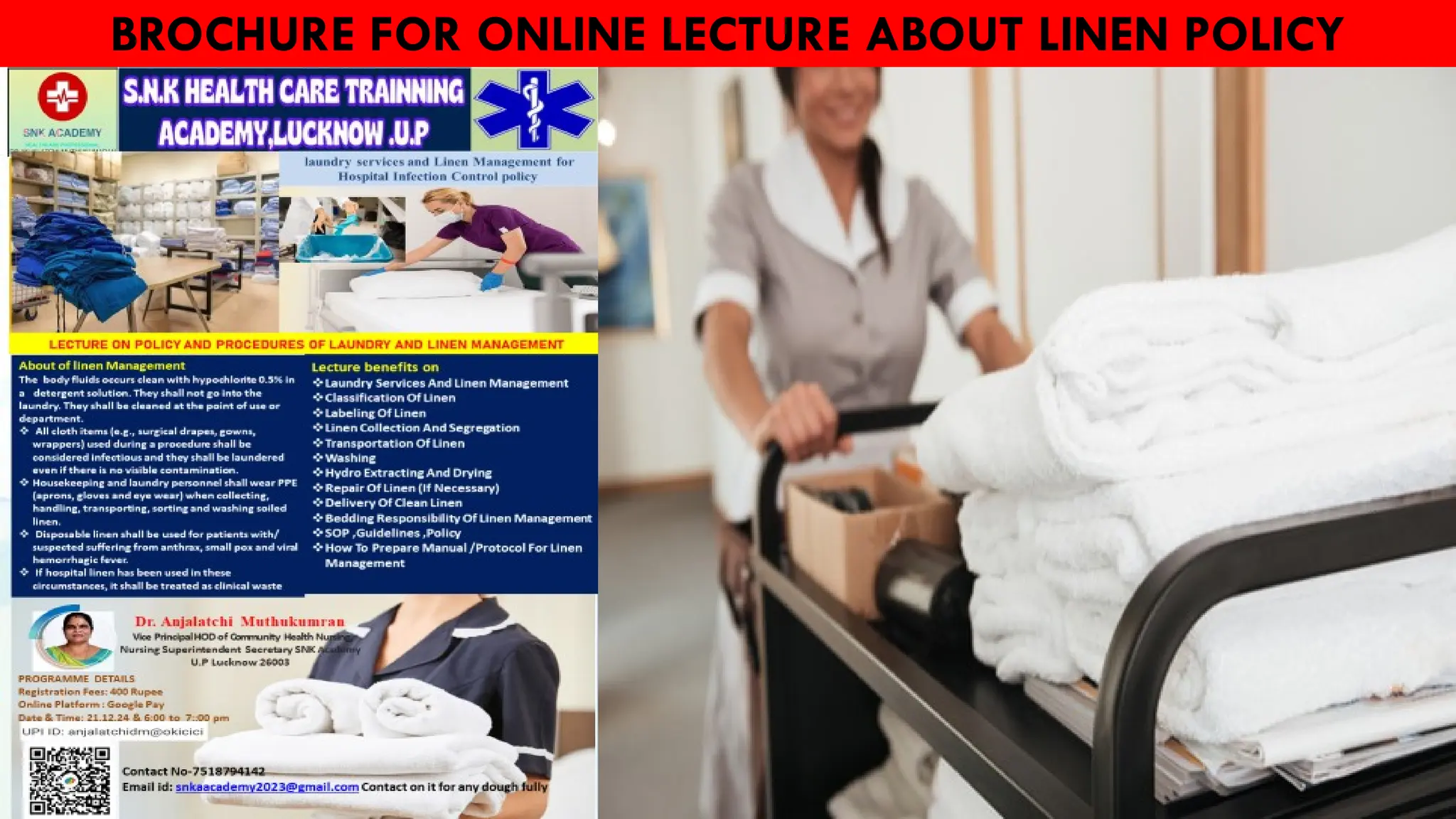
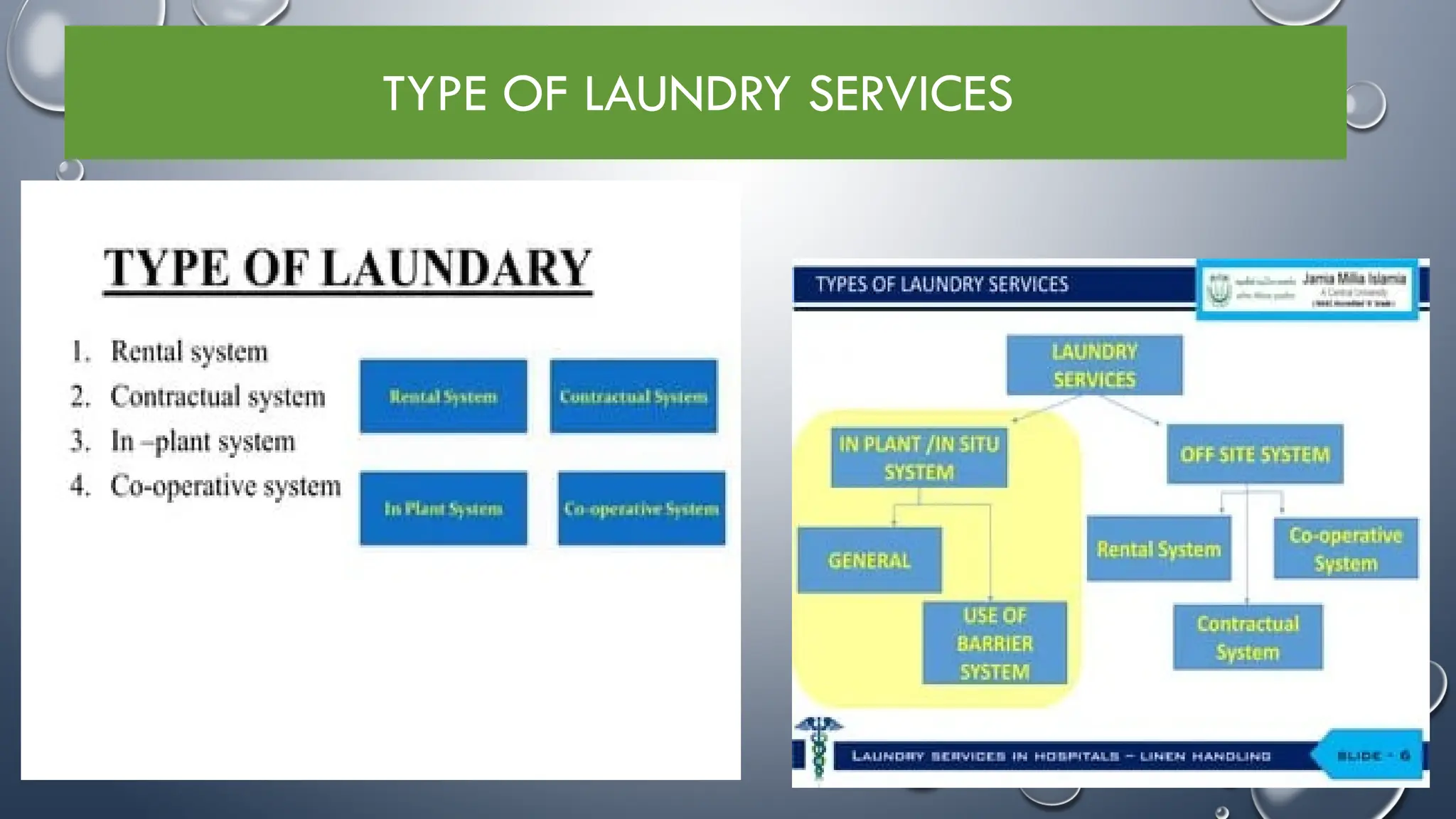
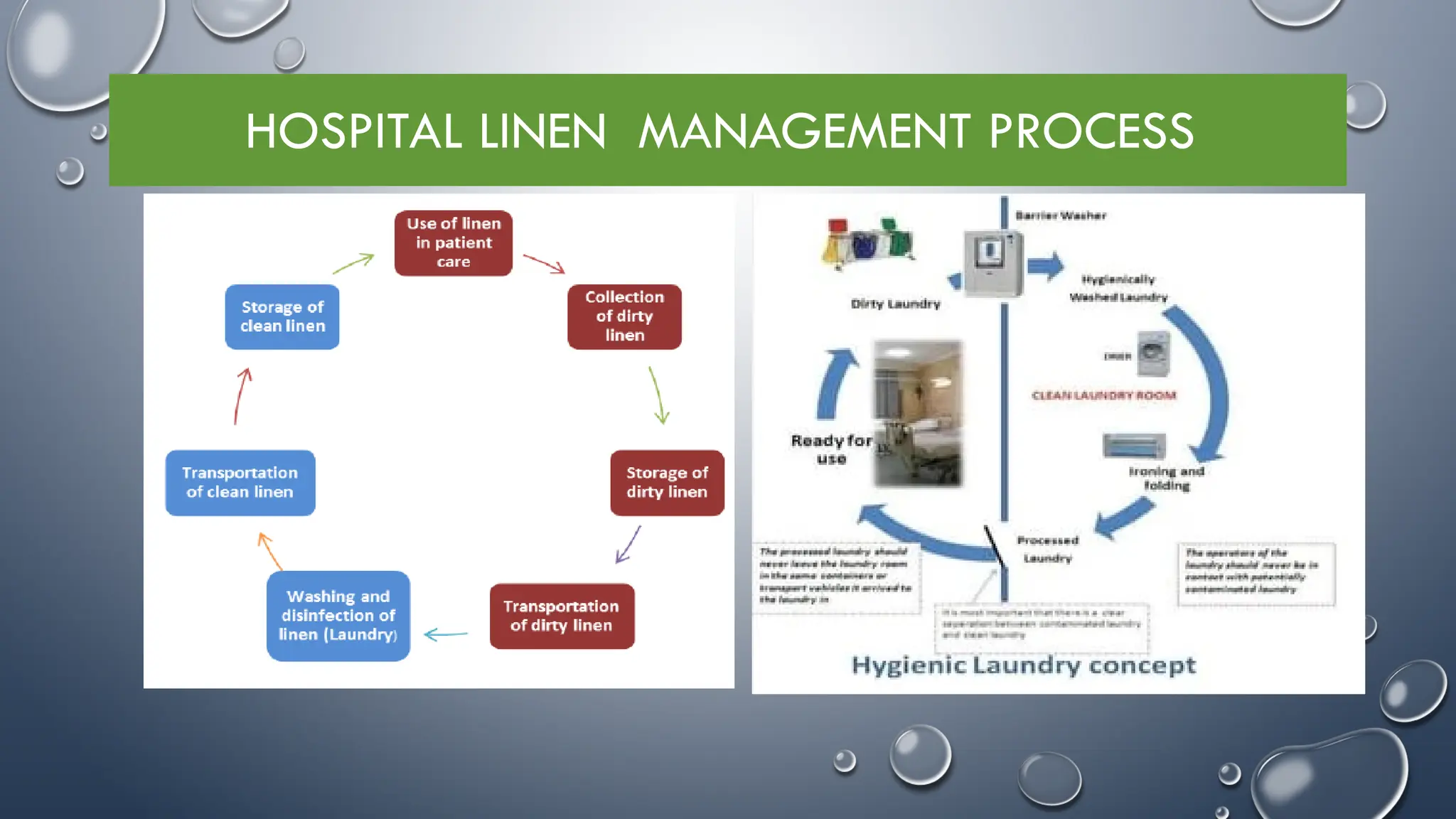
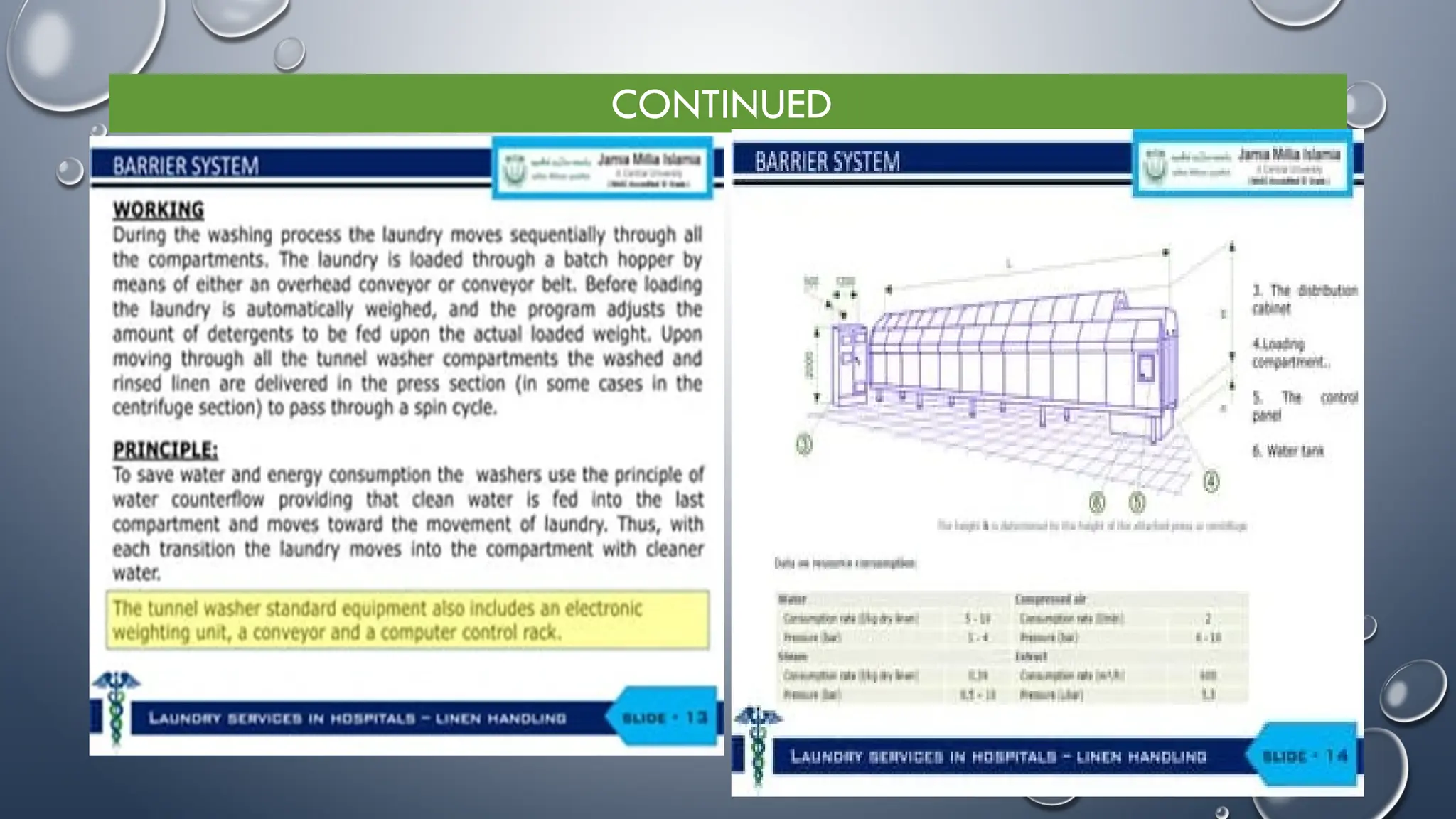
The document provides guidelines on laundry and linen management in hospitals, detailing types, classification, and handling procedures for various linen used in patient care. It emphasizes the importance of proper linen management to prevent infection risks and enhance hospital hygiene, including practices for collection, segregation, washing, and delivery of clean linen. Additionally, it outlines responsibilities of hospital staff and the necessity for recording and monitoring linen usage to mitigate losses.





















![ WASHING OF HOSPITAL LINEN PROCESS
• Washing By Hand
• STEP1: Wash Heavily Soiled/Infected Linen Separately From Non-
soiled Linen
• STEP 2: Wash The Entire Item In Water With Liquid Soap
• To Remove All Soilage, Even If Not Visible
REMEMBER: Pre-soak In Soap, Water And Bleach ONLY If Linen Is
Soiled-
Use Warm Water If Available
Add Bleach (For Example, 30–60 Ml [About 2–3 Tablespoons], Of A
5%chlorine Solution) To Aid Cleaning And Bactericidal Action
Add Sour (A Mild Acid Agent) To Prevent Yellowing Of Linen, If
Desirable
Step-3: Check The Item For Cleanliness. Rewash If It Is Dirty Or Stained
STEP 4: Rinse The Item With Clean Water](https://image.slidesharecdn.com/linenmanagmentppt2024-250101104629-72dc2154/75/Linen-Managment-services-in-hospital-ppt-2024-pptx-29-2048.jpg)